Steatosis/Steatohepatitis
– Mild steatosis (see comment)
COMMENT: The liver biopsy shows mild steatosis (approximately ***%). The portal tracts demonstrate minimal chronic inflammation. There is no significant interface activity. There is no significant lobulitis. No Mallory–Denk bodies are identified. Ballooning degeneration is not prominent. The bile ducts are normal in number and morphology. Overall, the findings are most consistent with mild steatosis. A trichrome stain does not demonstrate any significant fibrosis. Clinical correlation is recommended.
– Steatohepatitis (see comment)
COMMENT: The liver biopsy shows *** macrovesicular steatosis (approximately ***%). There is *** hepatocyte ballooning and a *** lobulitis. Mallory-Denk bodies are not identified. The portal tracts show *** chronic inflammation. The bile ducts appear to be normal in number and morphology. Overall, these findings are diagnostic of steatohepatitis, with the differential diagnosis primarily including non-alcoholic steatohepatitis (NASH) and alcoholic steatohepatitis, which often cannot be distinguished from one another histologically. Certain medications and rare genetic syndromes can also cause steatohepatitis. Assuming that this represents NASH, the steatohepatitis has a grade of ***. A trichrome stain demonstrates *** fibrosis consistent with a stage of ***. Clinical correlation is recommended.
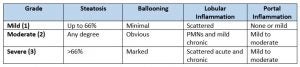
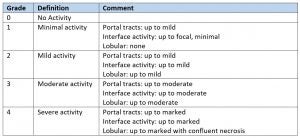
Grading & Staging steatohepatitis:
Modified Brunt System (Brunt EM. Semin Liver Dis. 2004 Feb;24(1):3-20. )
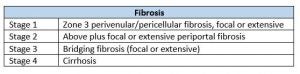
NASH CRN System (Kleiner DE et al. Hepatology 2005)
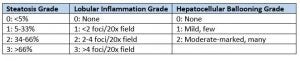
NAFLD activity score (NAS): 0-8 (Steatosis grade + Lobular inflammation grade + Ballooning grade)
Alcoholic Hepatitis
– Active hepatitis with extensive ballooning degeneration and bridging fibrosis, compatible with alcoholic hepatitis (see comment)
COMMENT: The liver biopsy shows extensive hepatocyte ballooning with lobular disarray and a lobulitis composed of primarily neutrophils with scattered lymphocytes. Numerous Mallory-Denk bodies are identified. There is mild steatosis (approximately 10%). The portal tracts demonstrate patchy inflammatory infiltrates and a mild bile ductular reaction. There is lobular and canalicular cholestasis. A trichrome stain demonstrates extensive pericellular fibrosis with areas of bridging fibrosis. Frank cirrhosis with nodule formation is not present.
Review of the medical record demonstrates a history of alcoholic hepatitis. Overall, these findings are consistent with alcoholic hepatitis. Clinical correlation is recommended.
Autoimmune Hepatitis
– Chronic Hepatitis, compatible with autoimmune hepatitis (see comment)
COMMENT: The liver biopsy shows a *** chronic hepatitis with dense portal infiltrates composed of lymphocytes and easily identifiable plasma cells. There is interface activity and hepatocyte regenerative rosette formation. There is a moderate chronic lobulitis. The bile ducts appear normal in number and morphology. Review of the medical record demonstrates that the patient has a positive anti-smooth muscle antibody, positive ANA, and elevated serum IgG. Together, the clinicopathologic findings are compatible with autoimmune hepatitis. A trichrome stain shows *** fibrosis. Clinical correlation is recommended.
Primary Biliary Cholangitis
– Chronic portal inflammation with bile duct destruction, compatible with Primary Biliary Cholangitis (see comment)
COMMENT: The liver biopsy shows a variable, moderate portal inflammatory infiltrate composed of primarily lymphocytes, with scattered plasma cells and rare neutrophils. There is no significant interface activity. Although several portal tracts show relatively normal-appearing bile ducts, many show lymphocytic bile duct inflammation and destruction. A possible portal granuloma is identified. There is no significant steatosis or lobulitis.
The patient’s history of a positive antimitochondrial antibody is noted. Overall, the histologic findings are most consistent with mild primary biliary cholangitis (previously called primary biliary cirrhosis). A trichrome stain demonstrates *** fibrosis. There are no histologic findings to support concurrent autoimmune hepatitis. Clinical correlation is recommended.
Active Hepatitis
– Active Hepatitis (see comment)
COMMENT: The liver biopsy shows extensive lobular disarray, hepatocyte ballooning, and lobular inflammation. The lobular infiltrate contains both lymphocytes and neutrophils. The portal tracts also demonstrate a moderate, mixed inflammatory infiltrate. There are areas of interface activity. Several bile ducts show infiltration by lymphocytes and there is a bile ductular reaction. Plasma cells are inconspicuous. There are multiple foci of spotty necrosis. Scattered acidophil bodies are identified. Reticulin and trichrome stains show areas of parenchymal collapse, without well-developed fibrosis. A PASD stain highlights numerous Kupffer cells. There are no globules to suggest alpha-1 antitrypsin deficiency. There is no significant steatosis or cholestasis.
Overall, these findings are most consistent with an active hepatitis. The primary differential diagnosis for this histologic pattern includes acute viral hepatitis and toxin/medication-related injury. Of note, there is no bland, coagulative-type central necrosis to suggest ischemic necrosis (“shock liver”) or acetaminophen toxicity. Additionally, no viral inclusions are identified to suggest adenovirus hepatitis or herpes hepatitis. These findings would also be somewhat unusual for autoimmune hepatitis and Wilson’s disease.
Sinusoidal dilation/ Outflow obstruction
– Sinusoidal dilation (see comment)
COMMENT: The liver biopsy shows diffuse sinusoidal congestion that is accentuated around central veins. There is no significant steatosis. There is associated hepatic plate atrophy. Portal tracts demonstrate minimal to no chronic inflammatory infiltrates. There is no significant lobulitis. The bile ducts appear normal in number and morphology. The trichrome stain does not demonstrate any significant fibrosis. There is trace stainable iron, primarily within sinusoidal macrophages.
Overall, the primary differential diagnosis includes hepatic venous outflow obstruction (e.g., due to right heart failure, hepatic vein occlusion, or inferior vena cava occlusion) and nodular regenerative hyperplasia. Clinical and radiographic correlation is recommended
(or, if they had congenital heart disease)
Overall, the findings are consistent with hepatic outflow obstruction, and could be compatible with the patient’s history of congenital heart defects. Clinical correlation is recommended
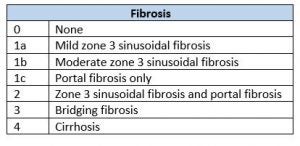
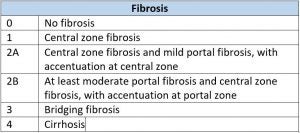
Fibrosis due to Hepatic Congestion Staging
Viral Hepatitis
– Chronic viral hepatitis C
– Grade *** activity, Stage *** fibrosis (see comment)
COMMENT: Histologic sections of the liver biopsy show a chronic hepatitis with *** portal inflammatory infiltrates composed of primarily lymphocytes. There is *** interface activity and *** lobulitis. There is *** necrosis. A trichrome stain demonstrates *** fibrosis.
Overall, the findings are compatible with the patient’s reported history of chronic viral hepatitis C with an activity grade of *** and a fibrosis stage of ***. Clinical correlation is recommended.
Batts-Ludwig System for Grading Chronic Hepatitis
Batts-Ludwig System for Staging Chronic Hepatitis
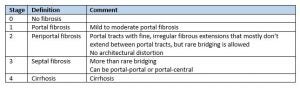
From: Batts KP, Ludwig J. Chronic hepatitis. An update on terminology and reporting. Am J Surg Pathol. 1995 Dec;19(12):1409-17.
Secondary Hemosiderosis
– Mild hemosiderosis (see comment)
COMMENT: The liver biopsy demonstrates deposition of iron within scattered sinusoidal Kupffer cells. There is very mild iron deposition within hepatocytes. This pattern of iron deposition is classically seen in secondary causes of iron overload such as transfusions, iron supplementation, and chronic renal dialysis. Otherwise, there is no significant fibrosis, steatosis, or inflammation
Resolving Hepatitis Pattern
– Scattered Kupffer cells (see comment)
COMMENT: The liver biopsy appears almost normal with no significant steatosis (less than 5%) and no significant fibrosis. Within scattered portal tracts, there are collections of ceroid-laden macrophages (Kupffer cells). Otherwise, there is minimal portal chronic inflammation.
The significance of these Kupffer cell aggregates is somewhat unclear, but may correlate with the patient’s history/clinical course as there are increased Kupffer cells in the setting of “resolving hepatitis,” with recent, but resolving injury. The most common causes of this pattern are acute self-limited viral infection and idiosyncratic drug reactions.
Other causes of elevated liver enzymes with essentially normal liver biopsies include systemic autoimmune conditions, vascular outflow obstruction, intermittent ischemia, medications, and even metabolic syndrome (which can sometimes contain minimal fat).
Clinical and serologic correlation is recommended.
Cirrhosis
– Cirrhosis (see comment)
COMMENT: Histologic sections of the liver biopsy show extensive fibrosis with regenerative nodule formation, consistent with cirrhosis. There is no significant steatosis (less than 5%). The fibrous septae show a bile ductular reaction and variable chronic inflammatory infiltrate composed of lymphocytes and plasma cells. Interface activity is not prominent. There is minimal lobulitis.
Overall, the etiology of the cirrhosis is somewhat unclear. Review of the medical record demonstrates a history of excessive alcohol use and obesity with negative viral hepatitis serologies. While the observed findings could be compatible with end-stage (“burnt out”) steatohepatitis, there are no definite histologic findings to confirm this etiology. Clinical correlation is recommended.
STAINS:
Trichrome: Shows bridging fibrosis with nodules, consistent with cirrhosis
Reticulin: Normal hepatic plate thickness
Iron: No stainable iron
PAS: Abundant glycogen stores
PAS-D: No globules to suggest alpha-1 antitrypsin deficiency
Last updated: 5/23/24